Acute pulmonary embolism: an update on management
Acute pulmonary embolism can be managed with thrombolysis, anticoagulation and newer interventional therapies. There is increasing evidence to guide the duration of anticoagulation and type of agent used, including warfarin, nonvitamin K antagonist oral anticoagulants and low molecular weight heparins.
- Treatment options for managing pulmonary embolism (PE) include anticoagulation and, in haemodynamically unstable PE, thrombolysis. It is less clear whether thrombolysis is of benefit in patients with submassive PE; in patients with lower-risk PE, anticoagulation alone is recommended.
- Duration of anticoagulation for PE is guided by risk of recurrence, risk of bleeding and, if appropriate, patient preference.
- Anticoagulation should continue for at least three months if PE was provoked by a transient risk factor; consider six months of anticoagulation if there is no obvious precipitant.
- Nonvitamin K antagonist oral anticoagulants (NOACs) are noninferior to vitamin K antagonists in most patients with PE, but there is no evidence regarding their use in massive PE or pregnancy.
- Aspirin is better than placebo for prevention of venous thromboembolism (VTE) recurrence, but standard-dose warfarin and NOACs are twice as effective as aspirin.
- Management of VTE during pregnancy should be with low molecular weight heparin (LMWH) for the remainder of pregnancy and until at least six weeks postpartum or three months in total.
- Patients with cancer benefit from LMWH over vitamin K antagonists in treatment of PE, possibly independent of PE risk.
- Inferior vena cava filters confer no additional benefit in patients who can tolerate anticoagulation for PE.
- Testing for heritable thrombophilias should not be routine after VTE.
Pulmonary embolism (PE) is caused by obstruction of the pulmonary arteries by thrombus, tumour, air or fat. Venous thromboembolism (VTE) including both PE and deep vein thrombosis (DVT) have a recurrence rate of 7% to 13% at 12 months.1-6 Overall, 25% to 50% of patients with first-time VTE do not have an identifiable risk factor. Fatal PE ranges from 0.01% among low-risk surgical patients to 5% among hospitalised medical patients with multiple risk factors.7,8 VTE is more than 100 times more common in the elderly than in children (500 cases per 100,000 persons at age 80 years vs five cases per 100,000 persons under 15 years of age).6
Acute PE is classified by the presence or absence of haemodynamic instability and markers of right ventricular (RV) strain, which reflect the severity of the PE and guide treatment options (Table 1).9
Clinical presentation and diagnosis of pulmonary embolism
Patients with acute PE typically present with chest pain, haemoptysis, tachycardia and/or dyspnoea, although symptoms can be very nonspecific.10 Risk factors for PE include increasing patient age, obesity, hospitalisation for surgery or acute illness, nursing-home confinement, active cancer, trauma or fracture, immobility or leg paresis, superficial vein thrombosis, and in women, pregnancy and puerperium, and oral contraception or hormone therapy use.11 Hypoxia in patients with PE is due to the mechanical obstruction to pulmonary vasculature causing ventilation-perfusion mismatch, atelectasis and surfactant dysfunction. Pulmonary vascular resistance increases with mechanical obstruction and hypoxia-induced vasoconstriction. This increases right heart pressures and can lead to acute right heart failure.
The Wells score is a clinical decision rule to stratify risk of PE (Table 2). In a primary care study of 598 patients, a Wells score of less than four with negative d-dimer safely excluded PE in 98.5% of patients and only failed to detect pulmonary emboli in 1.5% of patients.12
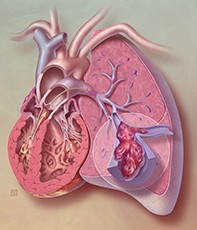
Chest x-rays are often normal in PE. A pulmonary infarction can occasionally be seen on chest x-ray as a Hampton hump, which is a dome-shaped, pleural-based opacification (Figure 1). PE can be diagnosed with CT pulmonary angiography, which is readily available and can reveal alternative diagnoses (Figure 2), or with ventilation-perfusion (V/Q) scanning, which exposes the patient (and particularly breast tissue) to less radiation. The sensitivity and specificity of V/Q scanning is comparable to CT pulmonary angiography in acute PE, but is less useful if the chest x-ray is abnormal, particularly in the presence of parenchymal lung disease.13,14 A transthoracic echocardiogram may show acute right heart strain in patients who are too unstable for definitive imaging, which in the correct clinical context would provide supporting evidence for a diagnosis of PE.15
Management of pulmonary embolism
Treatment options for managing PE include anticoagulation and, in haemodynamically unstable PE, thrombolysis.
Haemodynamically unstable pulmonary embolism
Thrombolysis in patients with massive PE associated with hypotension reduces mortality compared with anticoagulation without lytic therapy.9 In a prospective, randomised controlled study of eight patients with massive PE (which was terminated early), all four patients assigned to thrombolysis survived and all four patients in the anticoagulation-only group died.16 A 2014 meta-analysis of 2057 patients from 15 randomised trials compared thrombolysis with anticoagulation alone and also found a mortality benefit for thrombolysis therapy in massive PE.17 Thrombolysis may benefit patients with massive PE even in the context of cardiac arrest and in the immediate postoperative setting.18-20 In a study of 145 patients within three months of completed ischaemic stroke, and studies in 16 patients with low-grade intracranial neoplasms (such as meningioma), thrombolysis did not seem to result in a significantly higher risk of intracranial bleeding, although they are both relative contraindications to thrombolysis.21-23 Surgical embolectomy and catheter-directed interventions are options for patients who fail thrombolysis or whose risk of thrombolysis is too great.24-27
Haemodynamically stable pulmonary embolism
Submassive or intermediate-risk pulmonary embolism
How to manage patients with intermediate-risk PE is not as clear. Patients with submassive PE and elevated troponin levels have higher mortality (19.7%) compared with patients with normal troponin levels (3.7%).28 RV dysfunction seen on transthoracic echocardiogram in patients with intermediate-risk PE more than doubles their mortality risk.29 However, thrombolysis in this group does not improve overall mortality, as improved mortality from reducing RV dysfunction is offset by significant bleeding.30 Thrombolysis improves pulmonary haemodynamics and may lower the rate of acute and chronic pulmonary hypertension, but the clinical significance of this is unclear.9,31-33 Ongoing areas of study and debate include low-dose thrombolysis, restriction of thrombolysis to younger patients (<75 years) and catheter-directed thrombolysis.26,30,34,35
Low-risk pulmonary embolism
Patients who remain haemodynamically stable with normal biomarkers and a normal transthoracic echocardiogram should only be anticoagulated. Their short-term mortality is only 1% and they do not benefit from thrombolysis, which confers significant morbidity and mortality from bleeding.36
Use of nonvitamin K antagonist oral anticoagulants in acute pulmonary embolism
Nonvitamin K antagonist oral anticoagulants (NOACs) such as rivaroxaban, apixaban and dabigatran are noninferior to warfarin for acute treatment of VTE. They confer similar outcomes in VTE recurrence, fatal PE and overall mortality, with reduced rates of major bleeding.37
The dosages, reversal agents and pros and cons of using NOACs in patients with PE and the evidence for individual NOAC agents are summarised in Table 3.38-46 Important points to note about NOACs in PE are:
- Dabigatran is not PBS listed for PE or DVT therapy in Australia.
- NOAC therapy is guided by creatinine clearance as these drugs are largely renally excreted.
People with massive PE with haemodynamic instability were excluded from NOAC trials so there is no evidence to support the use of NOACs in such patients. There is also limited evidence for their use in patients weighing more than 120 kg and in pregnancy and malignancy.39,40-42
There are limited options for reversal of anticoagulation when using NOACs, although the TGA has approved idarucizumab as a reversal agent for dabigatran.47,48
There is a significant interaction between NOACs and p-glycoprotein inhibitors (such as ciclosporin and tacrolimus) and systemic antifungal medications (such as itraconazole and other azoles), leading to increased bleeding.49,50 There have been no head-to-head trials directly comparing the NOACs in acute VTE treatment.
Role of inferior vena cava filters in acute pulmonary embolism
Indications for use of inferior vena cava (IVC) filters are listed in Box 1.51-54 Inferior vena cava filter placement in addition to anticoagulation does not improve survival in patients with DVT except in those with haemodynamically unstable PE or after thrombolytic therapy.51,52 Insertion of filters increases the risk of recurrent DVT, an effect that offsets some of the benefits attributable to reduced PE.53,54
Treatment duration for PE
Treatment duration can be conceptualised in two phases:
- active treatment of the index event
- prevention of new episodes of VTE that are unrelated to the initial event.55
Active treatment of the index event
Three months of anticoagulation appears to suppress the acute episode of thrombosis as it was associated with a lower local recurrence compared with four to six weeks of anticoagulation.55-57 Patients with a large clot burden or unprovoked VTE may require six months of therapy.57
Prevention of recurrent VTE
The decision to continue anticoagulation after treatment for the index event is influenced by risk of recurrence, risk of bleeding, patient preference and associated complications such as post-thrombotic syndrome and pulmonary hypertension.
Risk of recurrence
Risk of recurrence is influenced by a variety of factors including provoking factors for the VTE (Table 4).56,58-62 In addition, an isolated distal DVT confers half the risk of recurrence compared with proximal DVT or PE.55 A second episode of VTE is associated with a 45% increase in recurrence at five years compared with a first event.57
To summarise, a first episode of isolated distal DVT provoked by surgery has a low risk of recurrence and the patient requires only three months of anticoagulation; however, a second episode of unprovoked VTE with high risk of recurrence requires at least six months and consideration of indefinite duration of anticoagulation in light of patient preference and bleeding risks.
Risk of bleeding
Risk of bleeding rises with increasing age. For each case of VTE complicated by major haemorrhage, the estimated case-fatality rate is 12%.63 Factors associated with increased bleeding during anticoagulation are listed in Box 2.63,64
There have been no randomised studies comparing placebo with indefinite anticoagulation in VTE with extended (10-year) follow up. The effect of indefinite anticoagulation on overall mortality from major haemorrhage, recurrent VTE and other causes is not clear.55 Studies examining extending anticoagulation in VTE prevention for an additional six to 18 months after a treatment period of six to 12 months and studies investigating adverse events associated with extended anticoagulation, particularly bleeding, would help guide management.
Aspirin (100 mg daily) was shown to reduce recurrent VTE by about one-third compared with placebo, without increasing bleeding risk, and also reduces cardiovascular risk.65 However, warfarin reduces this risk by more than 80%.64,66
Low-dose warfarin rather than standard- dose warfarin for prevention of recurrent VTE has been suggested as a possible compromise between recurrent VTE and bleeding risk. Although low-dose warfarin is better than placebo, conventional-dose warfarin is more effective at VTE prevention compared with low-dose warfarin, with similar bleeding risk in patients with two to four years of extended follow up.67,68
VTE recurrence was lower if a patient remained on indefinite (follow up nine to 48 months) anticoagulation (2.7%) compared with three to six months of therapy (18.8%) in a meta-analysis of four randomised studies.56,69,70-72 The incidence of major haemorrhage was higher in the indefinite anticoagulation group (4.6%) compared with the three-to-six-month group (1.5%).73 Other studies showed similar reductions in recurrent VTE using extended anticoagulation for an additional six to 12 months with dabigatran (150 mg twice daily), rivaroxaban (20 mg daily) and apixaban (2.5 mg twice daily).66, 74-77
A French study randomised 371 patients who had completed six months of warfarin for a first episode of unprovoked PE to placebo or anticoagulation with warfarin for an additional 18 months. Follow up was 42 months. The incidence of recurrent VTE was reduced during active therapy; however, this benefit was not maintained after discontinuation of anticoagulation therapy.78 The authors suggested that the initial VTE event had been adequately treated with six months of anticoagulation, but the underlying propensity for recurrent clotting was not modified by 18 months of extended anticoagulation.
Important subgroups at high risk of pulmonary embolism
Pregnancy and oestrogen exposure
Pregnancy increases the risk of VTE fivefold and oral contraceptives three- to fourfold.79-82 Use of oestrogen increases the risk of VTE 15-fold in the presence of Factor V Leiden.83,84 Use of oestrogen and progestin as hormone replacement therapy increases VTE risk twofold in low-risk women and five- to sevenfold in women at higher risk (due to older age and obesity).85 VTE risk in pregnancy increases with the presence of older age (over 40 years), obesity, pre-eclampsia and eclampsia, Caesarean delivery, multiple pregnancy, smoking, congenital and acquired thrombophilias, malignancy, hypertension and heart failure.86
Dyspnoea and leg swelling due to VTE during pregnancy are difficult to distinguish from the normal physiological symptoms of pregnancy. If PE is suspected, duplex ultrasound scanning of the legs should be performed after chest x-ray and ECG.87 If this is negative and clinical suspicion is high for PE, then V/Q scanning exposes the breast tissue to less radiation compared with CT pulmonary angiogram and is the preferred imaging modality in the presence of a normal chest x-ray.88 Radiation exposure is similar for the fetus. Clinical prediction rules such as the Wells score are not valid in the pregnant population so d-dimer is difficult to interpret.89
In pregnancy, treatment of established VTE consists of therapeutic doses of low molecular weight heparin (LMWH) or unfractionated heparin (UFH) given subcutaneously throughout the remainder of pregnancy and continuing to six weeks postpartum or until at least three months of treatment has been given in total.87,90,91
Warfarin is contraindicated during pregnancy as it crosses the placenta and is associated with miscarriage, teratogenicity and fetal and neonatal bleeding.91 Fetal exposure at six to 12 weeks’ gestation can cause a warfarin embryopathy characterised by nasal hypoplasia and/or stippled epiphysis.92 In the postpartum period, warfarin, UFH and LMWH are safe as they are not secreted into breast milk.91
Heparin-induced thrombocytopenia (HIT) develops in about 3% of nonpregnant patients treated with UFH, frequently complicated by extension of previous VTE or by arterial thrombosis.93 LMWH causes HIT less commonly than UFH, but should not be used when HIT has already been precipitated by UFH, as crossreactivity causes recurrent HIT. Danaparoid sodium is an effective alternative which does not cross the placenta and rarely produces recurrent HIT.93
The pharmacodynamics of LMWH change throughout pregnancy due to changes in volume of distribution and weight, so that periodic anti-factor Xa levels are recommended to guide therapy.91,94
Heparin during pregnancy does not increase rates of prematurity, abortions, stillbirths, neonatal deaths or congenital abnormalities,94 and major bleeding rates (2%) were similar to those among nonpregnant patients treated with warfarin and heparins.95
Malignancy
Cancer alone increases thrombosis risk 4.1-fold, and the addition of chemotherapy increases the risk 6.5-fold.96 Carcinomas of the pancreas, lung and stomach and adenocarcinomas of unknown primary site are the most strongly associated with thrombosis. LMWH appears to be superior to vitamin K antagonists in the treatment of VTE, with less bleeding and reduced recurrence of VTE.97-101 Cancer patients receiving therapeutic LMWH had improved survival in several prospective randomised trials, regardless of VTE presence.102-104
Travellers
People travelling by air for more than four to six hours have a two- to fourfold increased risk of VTE, especially in the two weeks after travel. There is no good evidence to guide use of pharmacological prophylaxis, but in those with high risk, such as previous VTE, recent major surgery (especially hip or knee surgery), pregnancy and malignancy, VTE prophylaxis can be considered.105
Further testing for inherited thrombophilia
About 5% of the population have a heritable thrombophilia that slightly increases their risk of VTE. However, most carriers do not experience DVT or PE.106 There are no studies evaluating the predictive value of heritable thrombophilia on recurrent VTE after modification of a precipitating risk factor, and duration of anticoagulation is influenced much more by clinical risk factors. Testing for heritable thrombophilia should not be routine after VTE and should only be undertaken after discussion about how it may alter management in selected clinical situations.107,108 Some guidance as to which patients might consider further testing for thrombophilias is given in Box 3.73
Conclusion
Thrombolysis improves mortality in patients with massive PE with haemodynamic compromise, but not in patients with intermediate-risk PE. Anticoagulation in most cases of VTE should be for three to six months, although the optimal duration for treatment and prevention of recurrence of PE is a subject for further investigation. NOACs are noninferior to VKA in most cases, and LMWH is useful in certain subgroups such as malignancy and pregnancy. Research into catheter-directed therapies is ongoing. CT