MINOCA. A new type of myocardial infarction
Patients with myocardial infarction with nonobstructive coronary arteries (MINOCA) sometimes remain unclear about whether they had an acute MI. Clinicians can assist by clarifying the underlying pathophysiology responsible for the ‘working diagnosis’ of MINOCA.
- Some patients with acute myocardial infarction (MI) do not have obstructive coronary artery disease; the term MINOCA (myocardial infarction with nonobstructive coronary arteries) was coined to describe such patients.
- MINOCA should be considered a ‘working diagnosis’ as ischaemic versus nonischaemic causes are initially delineated and the mechanism for the ischaemic infarction is subsequently identified.
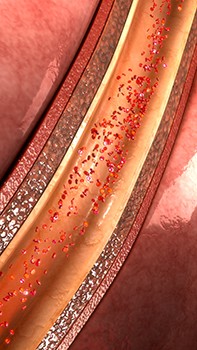
- Potential ischaemic causes are diverse, including coronary plaque disruption, occult coronary dissection, coronary thrombosis/embolism, coronary spasm (spontaneous or drug-induced) and coronary microvascular dysfunction.
- The underlying cause may influence the choice of therapy; however, use of conventional postinfarction cardioprotective therapies in patients with MINOCA is still under investigation.
Our understanding and, consequently, the management of acute myocardial infarction (MI) have evolved considerably over the past 100 years. In the early to mid 1900s, the focus of management was on reducing myocardial ischaemia by reducing myocardial oxygen demand, so patients were confined to bed with minimal exertion for six weeks. With the development of beta blockers, myocardial oxygen demand could be reduced pharmacologically rather than physically, and early (i.e. within a few days) mobilisation reduced the risk of pulmonary embolism.
In the 1960s, the advent of coronary care units for monitoring and treating patients with early infarction-related malignant arrhythmias (especially ventricular fibrillation) centralised clinical management and consolidated skills in managing acute MI, leading to a significant reduction in cardiac mortality.
In the 1980s, pivotal angiographic studies showed that almost 90% of patients with acute MI with ST elevation had an occluded infarct-related coronary artery, whereas only 32% of patients without ST elevation had an occluded artery.1,2 This resulted in the delineation of ST elevation MI (STEMI) and non-ST elevation MI (NSTEMI). In patients with STEMI, the strategy was to promptly restore coronary artery patency (the ‘open artery hypothesis’) in order to minimise MI size.3 This was initially achieved with thrombolytic therapy, but by the new millennium evolved into urgent percutaneous coronary intervention (PCI), which was more effective and associated with fewer major adverse events.4,5 The early treatment of NSTEMI has focused on antithrombotic therapy (preventing progression to a coronary occlusion), but the importance of early angiography to determine the extent of coronary artery disease has also become apparent.
The increased use of angiography in acute MI has also revealed that some of these patients do not have obstructive coronary artery disease. The term MINOCA (MI with nonobstructive coronary arteries) was coined to describe these patients, who present both a diagnostic and management puzzle for clinicians.6 Whereas patients with MI with obstructive coronary artery disease (MICAD) have an identifiable atherothrombotic mechanism to explain the acute MI, and therefore evidence-based management pathways, those with MINOCA do not. Thus, in patients with MINOCA, the underlying mechanism responsible for the acute presentation needs to be identified and therapies specifically targeting the underlying cause initiated.
Diagnostic criteria
As summarised in the Box, the diagnosis of MINOCA requires evidence of:
- acute MI
- no obstructive coronary artery disease – defined as <50% stenosis by convention
- no other overt cause for the acute presentation – particularly sepsis, pulmonary embolism or myocarditis.
Clinical features
The prevalence of MINOCA is estimated to be between 5 and 14%, with most contemporary large registries reporting about 10% prevalence among the population with acute MI.8,9 Based on a comprehensive systematic review comparing the clinical characteristics of patients with MINOCA to those with MICAD, the former were more likely to be younger and female, but less likely to have hyperlipidaemia.10 The VIRGO study, which focused on young patients (aged under 55 years) with acute MI, reported MINOCA to be five times more common in women than men.11 Furthermore, compared to patients with MICAD, these patients with MINOCA were less likely to have traditional cardiovascular risk factors, gestational diabetes or be postmenopausal but were more likely to have hypercoagulable states, use illicit drugs or have emotional stress or psychiatric illness (even after excluding takotsubo syndrome cases).11,12 However, social factors such as employment status and participation in sport did not differ between patients with MINOCA or MICAD.12 Studies in China and Korea described characteristics in patients with acute MI that were similar to those reported in European and North American cohorts.13,14
MINOCA – a working diagnosis
The contemporary definition of acute MI is centred on an elevated troponin level, with serial measurements confirming a rise and/or fall in levels, thereby indicating the acute nature of the presentation. Although troponin is the most specific cardiac biomarker clinically available for myocardial injury, it is not MI specific. Accordingly, other causes of myocardial injury besides ischaemic MI may result in troponin elevation.7
Acute myocarditis is the clinical condition that exemplifies this dilemma, since patients may present with chest pain, nonspecific changes on ECG and a raised troponin level with a subsequent rise or fall, mimicking MI. Although classic acute myocarditis may be easily distinguishable (i.e. young patient with an antecedent viral illness, presenting with pleuritic chest pain due to concurrent pericardial inflammation), in many patients it may be difficult to differentiate from MINOCA. Thus, MINOCA should be considered a ‘working diagnosis’ as ischaemic versus nonischaemic causes are initially delineated and the mechanism for the ischaemic infarction is subsequently identified.15,16
The Flowchart shows the diagnostic pathway for evaluating patients with suspected MINOCA. The initial approach should focus on differentiating nonischaemic causes of the elevated troponin level (i.e. causes of myocardial injury alone) from ischaemic causes. If the cause is ischaemic, a diagnosis of MI can be formally made.7 Myocardial injury resulting in an increased troponin level may arise from cardiac and extra-cardiac causes, which should be diagnosed by considering the clinical context of the troponin elevation. Cardiac MRI is a particularly useful investigation for differentiating cardiac causes of nonischaemic myocardial injury from true ischaemic MI. This imaging modality can differentiate myocarditis, MI and the takotsubo syndrome (or broken heart syndrome, which is especially prevalent in women17). Unfortunately, cardiac MRI is not readily available within the community, as access is largely limited to tertiary hospitals.
On confirming the presence of ischaemic-based infarction, thereby fulfilling the criteria for MINOCA, the ischaemic causes for the MI need to be considered. This may include diverse causes such as coronary plaque disruption, occult coronary dissection, coronary thrombosis or embolism, coronary spasm (spontaneous or drug-induced) and coronary microvascular dysfunction. The underlying cause may influence the choice of therapy, since plaque disruption may warrant initiation of statins, coronary thromboembolism may require anticoagulation therapy, and coronary spasm the use of calcium-channel blockers. Furthermore, whether conventional postinfarction cardioprotective therapies (e.g. aspirin, statins, beta blockers or angiotensin-converting enzyme inhibitors) should be utilised in MINOCA requires further consideration.
Prognosis
The absence of obstructive coronary artery disease may not necessarily confer a benign diagnosis in MINOCA. Although comparative studies indicate a more favourable prognosis for those with MINOCA than for those with obstructive coronary artery disease, an all-cause inhospital mortality rate of 0.9% (95% confidence interval [CI], 0.5 to 1.3%) and a 12-month all-cause mortality rate of 4.7% (95% CI, 2.6 to 6.9%) are cause for concern.10 A prospective study conducted by the Korean Acute Myocardial Infarction Registry reported that 12-month all-cause mortality rates in patients with MINOCA were equivalent to those in patients with single- or double-vessel coronary artery disease associated with an acute MI.14 Furthermore, two studies that compared patients with MINOCA with those with no previous history of MI or coronary artery disease reported a higher all-cause mortality rate and higher rate of major cardiac events in patients with MINOCA. Accordingly, postinfarction therapies that improve prognosis need to be considered.18,19
Potential therapies
Currently, there are no prospectively-designed randomised clinical trials specifically investigating the treatment of MINOCA. As alluded to above, consideration needs to be given to therapies that target the underlying pathological mechanisms as well as conventional cardioprotective therapies. Conventional cardioprotective therapies were studied in a retrospective analysis of the highly-acclaimed SWEDEHEART MI registry, which included 9,136 patients with MINOCA.9 By comparing major adverse cardiac events (MACE) during a mean follow-up period of 4.1 years among MINOCA patients who did or did not receive specific cardioprotective therapies, the investigators showed:
- a 23% reduction in MACE with statin therapy
- an 18% reduction in MACE with angiotensin-converting enzyme inhibitors or angiotensin receptor blockers (ACE-I/ARB)
- a nonsignificant 14% reduction in MACE with beta blockers
- no benefit with dual antiplatelet therapy.
A retrospective analysis of the CURRENT-OASIS 7 trial, which randomised 25,086 patients with acute coronary syndromes referred for early intervention to receive either double-dose or standard-dose clopidogrel, showed MINOCA patients did not benefit from the double-dose clopidogrel regimen.20 These nonrandomised data require confirmation with randomised clinical trial data.
The MINOCA-BAT trial – the first MINOCA randomised controlled trial
Assessing the benefits of conventional postinfarction cardioprotective agents in MINOCA is challenging since these drugs no longer have drug patents and are therefore of limited interest to industry sponsorship. Thus, alternative research designs and funding models need to be used to undertake randomised controlled trials with these agents. Registry-based randomised controlled trials (rRCT) in cardiovascular research have been pioneered by Swedish researchers, utilising the comprehensive SWEDEHEART registry.21 This approach utilises the infrastructure of an established clinical quality registry to recruit patients and collect the key study endpoints, thereby substantially reducing study establishment costs.
Using this approach, an international consortium of dedicated researchers has established the MINOCA-BAT trial, which seeks to assess the impact of ACE-I/ARB and/or beta blockers on MACE (defined as all-cause death, or readmission for MI, stroke or heart failure) in patients with MINOCA and preserved systolic left ventricular function (ejection fraction >40%). This registry-based, pragmatically designed, international, multicentre, open-label, randomised controlled trial with a two-by-two factorial design has recruited its first patients (Clinical Trials.com NCT03686696). With its pragmatic design, MINOCA patients will be recruited shortly after the diagnosis is established and followed by their usual treating clinician, and the MACE endpoints will be monitored within the registry infrastructure. Although the treatment is randomised, only the class of agent is specified (ACE-I/ARB and/or beta blocker), with the specific agent being at the discretion of the treating clinician. For example, a patient randomised to beta blocker therapy may be prescribed atenolol (study preference) but could equally receive metoprolol. This pragmatic design allows:
- flexibility between study countries, where different beta blockers are often used
- choice for the treating clinician in prescribing therapies they are familiar with
- a ‘real world’ approach, since a demonstrated benefit with beta blockers will translate to increased use of this class of agents rather than a specific agent.
This novel rRCT approach represents the future of clinical trials, considering the spiralling costs of this multimillion-dollar industry. Furthermore, positive findings can be readily translated into routine clinical practice using the registry infrastructure. Advancing the diagnosis and treatment of MINOCA has only been plausible using this pragmatic approach and the support of treating clinicians.
Conclusion
MINOCA is an intriguing condition that is often overlooked and undertreated. The absence of obstructive coronary artery disease on angiography despite the diagnostic hallmarks of an acute MI often results in the patient being confused as to whether they did or did not have an acute MI. By making a diagnosis of MINOCA, and therefore flagging the need to identify the underlying pathophysiology responsible for this presentation (i.e. ‘working diagnosis’), clinicians can assist in clarifying the diagnosis for patients. In the future, clinical trials that are currently in progress (e.g. MINOCA-BAT Trial), will provide insights into the most appropriate discharge therapy for these patients.